Description
There are numerous types of brain tumours and they all behave differently and so require different combinations of treatment. Following is a brief account of the more commonly encountered tumours and our current thoughts on treatment.
Brain tumours can cause many different symptoms including (but not exclusively):
- Seizures (fits)
- Headaches
- Loss of use of your arm or leg
- Inability to speak
- Decreased vision, double vision
- Confusion
Sometimes brain tumours can be found incidentally on scans performed for unrelated symptoms.
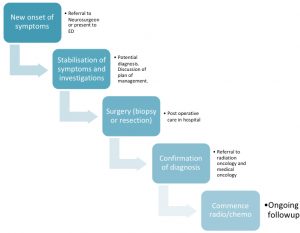
Below is a flow chart of what happens to patients when they are diagnosed with a brain tumour.
Commonly Occurring Brain Tumours
Gliomas
Gliomas are primary brain tumours. They arise from the supporting cells of the brain. The two main types of gliomas are Astrocytomas and Oligodendrogliomas. Rarer types are Ependymomas and Choroid plexus tumours.
We do not know what causes these tumours. Radiation exposure can give rise to these tumours. However the vast majority of patients who have gliomas have never had significant radiation exposure. There is some debate at present about the effect of mobile phones. We do not have firm evidence for this and the current thinking is that there is no link.
Some people with certain genetic conditions also develop gliomas.
Gliomas are graded by the WHO ( World Health Organization) from 1-4. The grade gives us an idea of how quickly it is growing and spreading and so also helps guide treatment.
Grade 1 is considered benign. Grade 2 is also called “low grade” and implies a slow growth rate. However a grade 2 tumour can subsequently progress to become a grade 3 or 4.
Grade 3 and 4 tumours are considered malignant and rapidly growing. The grade 4, also called Glioblastoma, is the most aggressive type.
Apart from a grade 1 which can be cured with surgery, the other grade tumours do not have a cure at present. Treatment generally involves a combination of surgery, radiotherapy and chemotherapy which are all aimed at slowing down the growth and spread of these tumours. Many clinical trials are now becoming available for the trial of new novel treatments.
Prognosis (with treatment):
Grade 1 – Excellent. Potentially curable
Grade 2 – Good. Long term survival over many years.
Grade 3 – Guarded. Long term survival over a few years.
Grade 4 – Poor. Average survival around 16-18months.
Meningiomas
Meningiomas are benign slow growing tumours that arise from the lining of the brain called the Dura. Some of them can be more rapidly growing or malignant.
At this point in time we have no known cause. However, certain previous radiation to the head, increases the risk of formation of these tumours. They are also more common in women and so may respond to female hormones.
They can arise anywhere within the skull and spine. As they arise from the membrane that contains the brain and spine, they are on the surface and press on the brain or spine. Rarely they can arise within the ventricles (fluid cavities)
Treatment for meningiomas depends on various factors:
- Size
- Location
- Symptoms
- Age and general condition of patient
Treatment options are
- Watch and wait
- Surgery alone
- Surgery and radiation
- Radiation alone
Prognosis :
Meningiomas are graded by the WHO (World Health Organisation) to give us a guide as to how quickly they grow.
Grade I – 90% of meningiomas. These are very slow growing and on average grow 1-2mm per year. Execellent prognosis. Often cured with just surgery alone.
Grade II – 8%. Also called atypical meningiomas. More rapidly growing and greater tendency to recur after surgery. Guarded prognosis.
Grade III – 2%. Also called malignant meningioma. Rapidly growing and invades brain and can also spread throughout the brain and elsewhere. Poor prognosis.
Pituitary Tumours
Pituitary tumours are benign slow growing tumours called adenomas. They arise from the pituitary gland which is the hormone control centre of the brain and is located at the base of the brain.
These tumours sometimes produce an excess of hormone and so are called functional tumours. The most common syndromes caused by hormone excess are Prolactinoma, Cushings Disease, and Acromegaly.
Non functional tumours often grow to quite a large size and cause symptoms relating to vision as they exert pressure on the optic nerves.
Treatment
Before surgery, all patients need to see an endocrinologist (hormone specialist) and have their vision formally assessed.
Most pituitary tumours then require surgery and occasionally drug treatment or radiotherapy. Prolactinomas are usually treated with drugs.
Surgery is generally performed endoscopically via the nose.
Prognosis
Generally good as these are benign tumours.
Brain Metastases
Malignant tumours that arise elsewhere in the body may secondarily seed in the brain.
Malignant tumours shed cells that can enter the blood stream. At any one time, a quarter of our total blood volume is in the brain. This makes the brain a common site for secondary brain tumours. There may be only one tumour in the brain or many.
In Australia we have a very high incidence of melanoma and so there is a high incidence of metastatic melanoma to the brain. Other cancers that seed in the brain are breast, lung and colon.
Treatment
Treatment of brain metastases is complicated and discussion is needed between various specialists to determine the best course of action. This is called a Multi Disciplinary Team (MDT) approach.
Treatment generally involves a combination of surgery, radiotherapy and drug treatment. The drug treatment is different for different cancers.
At present, there are a growing number of treatments available and also clinical trials, which have resulted in a much improved prognosis for many cancers.
Some of the Brain Tumour/Cancer research we have funded
In 2022 Dr Stanley Stylii was the recipient of Brain Foundation grant funding – click for more.
In 2019 Dr Ayenachew Bezawork-Geleta was the recipient of Brain Foundation grant funding – click for more.
In 2019 Dr Jordan Jones was the recipient of Brain Foundation grant funding – click for more.
In 2018 Dr Iman Azimi was the recipient of Brain Foundation grant funding – click for more.
In 2018 Dr Mastura Monif was the recipient of Brain Foundation grant funding – click for more.
For further information and support
http://www.brain-surgeon.com.au/brain-tumours/
Click here for the latest Australian research papers on Brain Tumour and Brain Cancer.
The Cancer Council NSW
PO Box 572, Kings Cross NSW 1340
Ph (02)9334 1900
cancercouncil.com.au
The Cancer Council Victoria (with links to Cancer Councils in all states)
1 Rathdowne Street, Carlton VIC 3053
Ph (03) 9635 5000
Fax (03) 9635 5270
Email enquiries@cancervic.org.au
www.cancervic.org.au/about-cancer/cancer_types/brain_tumour/
Brain Tumour Alliance Australia (BTAA)
PO Box 717, Mawson, ACT 2607
Ph 1800 857 221
Email btaa@shout.org.au
BTAA has a support group that meets in Sydney once a month
www.btaa.org.au
BTAA Sydney Support Group
https://www.facebook.com/groups/1752312241691477/
James Crofts Hope Foundation (WA)
PO Box 112, Innaloo WA 6918
Ph 0428 247 319 (Secretary)
Email info@jamescroftshopefoundation.org.au
www.jamescroftshopefoundation.org.au
Reviewed March 2018 by Dr Brindha Shivalingam, Director of Neurosurgery, The Chris O’Brien Lifehouse.
DISCLAIMER: The information provided is designed to support, not replace, the relationship that exists between a patient / site visitor and his / her existing health care professionals.




 The Brain Foundation is the largest, independent funder of brain and spinal injury research in Australia. We believe research is the pathway to recovery.
The Brain Foundation is the largest, independent funder of brain and spinal injury research in Australia. We believe research is the pathway to recovery.