Chronic traumatic encephalopathy (CTE) is a type of dementia associated with repeated head injuries or concussions. It is often discussed in relation to contact sports, but it can occur in anyone who suffers from repeated head traumas.
There is currently no cure for CTE, but researchers are working hard to change this. In the meantime, many researchers and advocates are pushing for increased awareness about the risks of concussion & head injuries to help prevent CTE.
Click on the headings below to jump to a specific section.
- What is chronic traumatic encephalopathy?
- Definitions & key terms
- Symptoms
- Causes
- Diagnosis
- Current research
- Treatment
- Prognosis
- Further information & resources
Medically reviewed by Dr Alan Pearce and A/Prof Michael Buckland. Last updated October 25, 2023.
What is chronic traumatic encephalopathy?
Chronic traumatic encephalopathy (CTE) is a type of neurodegenerative disease associated with repeated head injuries, concussions or subconcussions. It was first identified in boxers in the 1920s and was called ‘punch drunk syndrome’ or ‘dementia pugilistica’. Recently it has been discussed in relation to other contact sports such as rugby, Australian rules football, and soccer.
Like other types of neurodegenerative diseases, CTE causes a wide range of symptoms, often relating to thinking, mood and behaviour. However, symptoms can begin much earlier than a disease like Alzheimer’s disease. Cognitive and behavioural (mental health) symptoms might begin in a person’s 20s or 30s. Comparatively, Alzheimer’s disease might not be symptomatic until your 80s.
While CTE is most commonly associated with contact sports, it has been recognised in a variety of other athletes and individuals who have experienced repeated head traumas. It is important to note that not everyone who experiences repeated head injuries will develop CTE.

Definitions & key terms
| Concussion | Concussion is a common type of mild traumatic brain injury that occurs when the brain is shaken or jolted inside the skull. The impact causes brain strain with resultant inflammation, damage to nerve fibres, and a change in your metabolic state. Your brain suddenly releases neurotransmitters that can either overstimulate or inhibit brain function, and there may be microscopic bleeding with a loss of brain cells. |
| Subconcussion | A subconcussion refers to head injuries that do not result in the clinical symptoms of a concussion but can carry less, equal or greater force than a concussion. Some researchers now use the term ‘non-concussive impacts’ to refer to these mild brain injuries. Individually, these injuries seem minor because the person won’t show any noticeable symptoms. However, repeated subconcussions can compound over time and cause cumulative injury to the brain. |
| Encephalopathy | A broad term referring to any disease that affects the whole brain and alters its structure or how it works, and causes changes in mental function. The word is derived from ancient Greek - ‘encephalo’ meaning brain, and ‘pathos’ meaning suffering. |
| Pathology | The science of the causes and effects of diseases, especially the branch of medicine that deals with the laboratory examination of samples of body tissue for diagnostic or forensic purposes. |
| Neuropathology | A specialised type of pathology focused on diseases of the nervous system. In this article, neuropathology is relevant because researchers analyse brain tissue to diagnose CTE. |
| Tau protein | Tau protein is most commonly found in brain cells (neurons). Tau is important because it helps stabilise the microtubules or ‘internal skeleton’ of the neuron. The dysfunction of tau proteins is associated with many different brain diseases. |
| Neurofibrillary tangles | Neurofibrillary tangles are abnormal accumulations of tau proteins. Rather than sticking to the microtubules, tau proteins clump together and form tangles, which prevents the neuron from functioning properly. |
Symptoms of chronic traumatic encephalopathy
Chronic traumatic encephalopathy affects individuals differently, but there are common symptoms that many people experience. These symptoms often develop years or even decades after the initial head injuries and can progress over time. Symptoms could include (1,2):
- Cognitive symptoms. Memory loss, executive dysfunction, attention & concentration difficulties, language impairment, difficulty with vision/spatial perception.
- Behavioural symptoms. Explosivity, physical or verbal violence, “out of control” behaviour, impulse control problems, paranoia, being socially inappropriate.
- Mood-related symptoms. Sadness/depression, suicidal ideation or attempts, hopelessness, substance abuse, anxiety/agitation, manic behaviour, apathy.
- Motor symptoms. Parkinsonism i.e. tremors, impaired balance or coordination, abnormal gait such as limping, weakened vocal muscles which could cause slurred speech (dysarthria).
- Related movement disorders. Some people develop motor neurone disease (MND) or Parkinson’s disease in association with CTE (5).
Researchers identified these symptoms by interviewing family members of people who were confirmed to have CTE (1). This is because CTE can’t currently be diagnosed while a person is alive. The diagnosis is only confirmed by looking at the person’s brain tissue after they have passed away.
Research has also suggested that there are possibly two clinical presentations of CTE. Some people experience behavioural and mood symptoms first, while others experience cognitive symptoms first. There’s a significant difference in the age of onset between these two groups, and the duration of the disease.
Different presentations of CTE (1)
| Initially showing behavioural / mood symptoms (n = 22) | Initially showing cognitive symptoms (n = 11) | |
|---|---|---|
| Age when first symptoms were noticed | 34.5 years old (standard deviation 19 - 59) | 58.5 years old (standard deviation 31 - 82) |
| Duration of disease | 17.0 years (standard deviation 0 - 51) | 10.7 years (standard deviation 1 - 30) |
The variation in CTE is partially the reason that it is difficult to diagnose. If someone develops symptoms of depression and anger issues in their 20s or 30s, it may be misdiagnosed as a psychiatric disorder. On the other hand, if they have issues with memory loss later in life, it could be misdiagnosed as Alzheimer’s disease.
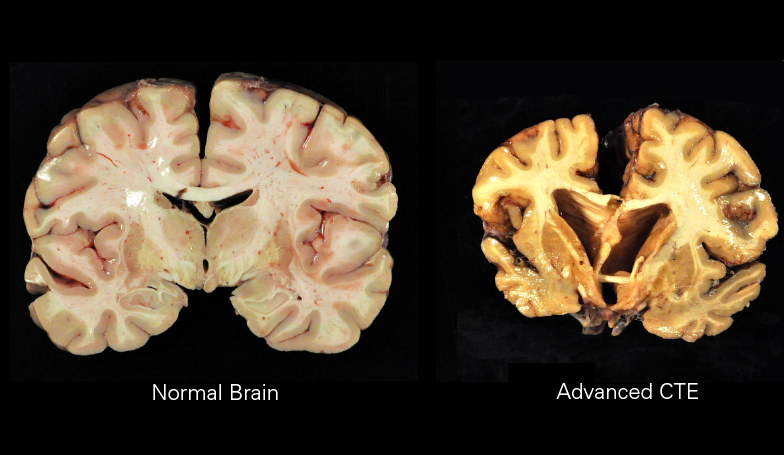
Causes
Chronic traumatic encephalopathy is not fully understood, but research has established a clear link between repetitive concussive or subconcussive blows to the head and CTE (2,7). When the brain experiences a trauma, it can cause a build-up of a protein called tau. Tau is a protein that, in its normal form, helps to stabilise the structure of nerve cells (neurons) in the brain. However, in CTE, tau becomes abnormally folded and forms clumps inside neurons, leading to cell death and brain atrophy (shrinkage).
These injuries are associated with:
- Contact sports such as rugby, Australian rules football, American football, wrestling, soccer, etc
- Other sports involving falls such as horseback racing
- Military veterans
- People with epilepsy (depending on the type & frequency of seizures)
- Victims of domestic abuse
This is not an exhaustive list – anyone who suffers repeated head trauma, regardless of the circumstances, carries a risk of developing CTE. However, there is no clear consensus on how much or little trauma is needed to cause CTE (2).
Diagnosis
Diagnosis of chronic traumatic encephalopathy is challenging because the symptoms often overlap with other neurological conditions such as Alzheimer’s disease, Parkinson’s disease, or depression. Currently, a definitive diagnosis of CTE can only be made post-mortem, by examining brain tissue during an autopsy.
However, there are guidelines for diagnosing traumatic encephalopathy syndrome (TES), which is the clinical disorder associated with neuropathologically diagnosed CTE. The diagnostic criteria were last updated in 2021 by a panel of 20 expert clinician-scientists in neurology, neuropsychology, psychiatry, neurosurgery, and physical medicine and rehabilitation (3). The diagnostic criteria are outlined in the diagram below.
Stepwise Process for Using the NINDS Consensus Diagnostic Criteria for Traumatic Encephalopathy Syndrome (3)
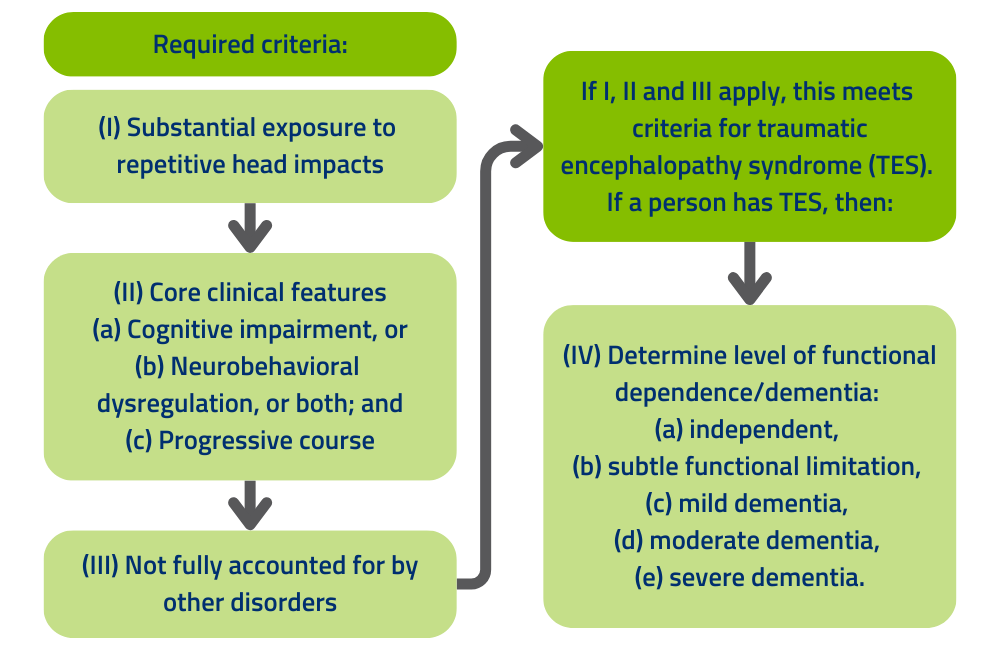
Doctors may use a combination of medical history, physical examination, and neuroimaging (e.g., MRI or CT scans) to assess the likelihood of CTE and rule out other possible causes of symptoms.
After a confirmed diagnosis of TES, there are further guidelines to estimate the level of certainty for CTE pathology. The levels of certainty include suggestive of CTE, possible CTE, probable CTE, and definite CTE (confirmed at post-mortem). You can view the full criteria in the original study, which is available for free via the National Library of Medicine >
Neuropathology & post-mortem diagnosis
Since 2011, numerous studies have proposed guidelines for post-mortem CTE diagnosis (3). Researchers needed to identify the markers that were specific to chronic traumatic encephalopathy rather than other neurodegenerative diseases such as Alzheimer’s disease.
A group of researchers published the diagnostic criteria following a consensus meeting in 2015 (4). This was a huge step forward for clinicians, patients and researchers, because it meant that people working in brain banks across the world could be on the lookout for CTE. A few neuropathological markers of CTE include (4):
- Abnormal tau proteins. Tau is involved in many different diseases, but the consensus panel found that the tau pathology in CTE is distinct from other diseases. In CTE, tau aggregates around small blood vessels, deep in the folds of the cerebral cortex.
- Neurofibrillary tangles. These tangles are found in different regions of the brain compared to Alzheimer’s disease and other dementias.
- Larger structural changes in the brain. In some cases parts of the brain will be shaped abnormally, or show other physical signs of traumatic brain injury.
These are just a few factors that scientists look for when diagnosing CTE, but the full process is much more complex.
If you are interested in donating your brain for CTE research, please consult the resources at the bottom of this page, or visit our page about how to donate your brain >
Current research
Research on chronic traumatic encephalopathy is ongoing, and scientists are working to better understand the disease and develop ways to diagnose and treat it. Some of the key areas of research include:
- Biomarkers: Researchers are trying to identify biomarkers (substances in the body that can be measured to indicate the presence or progression of a disease) that could help diagnose CTE in living individuals.
- Risk Factors: Understanding the risk factors for developing CTE is crucial for prevention. Current research is focused on determining how the number, severity, and frequency of head injuries are related to the risk of developing CTE.
- Treatment: There is currently no cure for CTE, so research is focused on developing treatments to manage symptoms and slow disease progression.
In 2023, there was a senate inquiry into concussions and repeated head trauma in contact sports. The report from this inquiry called for further research in relation to CTE and included statements from many of Australia’s top concussion & CTE researchers. You can read the full report on the APH website >

Australian research into chronic traumatic encephalopathy
The Australian Sports Brain Bank (ASBB) is an Australian research centre focusing on chronic traumatic encephalopathy. Since the ASBB was established in 2018, they have received more than 600 donation pledges from amateur and professional sportspeople (6). A donation pledge is when someone registers to donate their brain after they pass away, similar to organ donation.
In 2022 they published a paper about the first three years of research at the ASBB. Some of their updates included (6):
- They have received and studied the brains of 21 donors, all of whom had participated in sports with risks of repetitive head injury.
- All but one donor exhibited some form of neurodegeneration, and the most frequent neuropathology was CTE (12 donors).
- The proportion of professional participants was higher in the CTE group (67% vs 50%).
- Six of the 12 donors with CTE and one of nine without CTE had died by suicide, suggesting CTE may be a suicide risk factor.
If you are interested in reading the full paper, it is an open access article available via Wiley Online Library >
Treatment
Currently, there is no specific treatment or cure for chronic traumatic encephalopathy. Researchers instead focus on preventive measures, such as finding ways to reduce head injuries (2). In contact sports this might involve educating coaches, players and parents about the risks, ensuring that field medics know the signs of concussion, and penalising players for dangerous moves. Learn more about preventing concussion >
However, once a person has developed symptoms of CTE, treatment is focused on symptom management and strategies to improve the person’s quality of life. Some common treatment approaches include:
- Medication: Medications may be used to manage specific symptoms such as depression, anxiety, or sleep disturbances.
- Physical Therapy: Physical therapy can help manage motor problems such as difficulty with movement, coordination, or balance.
- Occupational Therapy: Occupational therapy can help individuals with CTE manage daily activities and maintain their independence.
- Cognitive Rehabilitation: Cognitive rehabilitation can help manage problems with memory, attention, and problem-solving.
It is important to note that while these treatments can help manage symptoms, they do not cure the disease or stop its progression.
Prognosis
The prognosis for chronic traumatic encephalopathy varies from person to person and depends on several factors including the severity of the disease, the age at which symptoms first appear, and the presence of other medical conditions. In general, CTE is a progressive disease that tends to worsen over time. However, the rate of progression and the severity of symptoms can vary widely among individuals.
Further information & resources
In 2019, Dr Claire Shepherd received a Brain Foundation research grant for her project Chronic Traumatic Encephalopathy >
If you’d like to learn more about chronic traumatic encephalopathy, the Brain Foundation or related topics, here are some further resources:
- Recent Australian CTE research – access via the PubMed database
- Concussion – our article providing an overview of concussion
- CTE Fact Sheet – a shortened version of this article is available as a downloadable PDF for printing.
- Donate your brain – information on different brain banks in Australia
- Concussions and repeated head trauma in contact sports (2023) – Senate Inquiry report
- Concussion Interview – Brett Kearney (retired NRL star) interviewed Dr Rowena Mobbs (leading concussion & CTE researcher) about concussion as part of Migraine & Headache Awareness Week 2023.
- Newsletters – subscribe to receive the Brain Foundation newsletter
Helpful organisations & services
Australian Sports Brain Bank
The Australian Sports Brain Bank’s mission is to use expert diagnostic neuropathology, coupled with research, to understand chronic traumatic encephalopathy (CTE) and other brain pathology that is associated with repetitive head injury in sport and elsewhere. They empower families and loved ones by providing accurate diagnoses, and use donor tissue for biomedical research into CTE and other brain disorders.
Email: info@brainbank.org.au
Tel: (02) 9351 0943
www.brainbank.org.au
Concussion Connect – Macquarie University
Concussion Connect is a neurology and psychology group therapy program for those suffering the effects of repeated head injury, with risk of chronic traumatic encephalopathy (CTE).
Email: neurology@mqhealth.org.au
www.mqhealth.org.au/services/wellness-services/concussion-connect
Dementia Australia
An organisation that represents the more than 400,000 Australians living with dementia and the more than 1.5 million Australians involved in their care. They provide a range of support services, informative resources, awareness events, advocacy programs, and more.
National Dementia Helpline: 1800 100 500
www.dementia.org.au/about-dementia/types-of-dementia/chronic-traumatic-encephalopathy-dementia
ConneCTErs Australia
This organisation provides support and community to people who have been affected by CTE. It was founded by Kayleen Doyle after her husband was provisionally diagnosed with CTE.
Email: hello@connecters.org.au
connecters.org.au
Synapse – Australia’s Brain Injury Organisation
Synapse provides a range of support services for people who have been impacted by brain injury and disability. These services promote quality of life, self-determination, and choice through information, specialist support, and targeted research activities.
Email: info@synapse.org.au
Tel: 1800 673 074
synapse.org.au/fact-sheet/chronic-traumatic-encephalopathy
References:
- R A Stern et al, 2013, Clinical presentation of chronic traumatic encephalopathy. DOI: 10.1212/WNL.0b013e3182a55f7f
- M Saulle & B D Greenwald, 2012, Chronic Traumatic Encephalopathy: A Review. DOI: 10.1155/2012/816069
- D Katz et al, 2021, National Institute of Neurological Disorders and Stroke Consensus Diagnostic Criteria for Traumatic Encephalopathy Syndrome. DOI: 10.1212/WNL.0000000000011850
- A C McKee et al, 2015, The first NINDS/NIBIB consensus meeting to define neuropathological criteria for the diagnosis of chronic traumatic encephalopathy. DOI: 10.1007/s00401-015-1515-z
- A C McKee et al, 2010, TDP-43 proteinopathy and motor neuron disease in chronic traumatic encephalopathy. DOI: 10.1097/nen.0b013e3181ee7d85
- C M Suter et al, 2022, Chronic traumatic encephalopathy in Australia: The first three years of the Australian sports brain bank. DOI: 10.5694/mja2.51420
- M E Buckland et al, 2022, Chronic traumatic encephalopathy as a preventable environmental disease. DOI: 10.3389/fneur.2022.880905
DISCLAIMER: The information provided is designed to support, not replace, the relationship that exists between a patient / site visitor and his / her existing health care professionals.





 The Brain Foundation is the largest, independent funder of brain and spinal injury research in Australia. We believe research is the pathway to recovery.
The Brain Foundation is the largest, independent funder of brain and spinal injury research in Australia. We believe research is the pathway to recovery.