Multiple Sclerosis (MS) is one of the most common acquired chronic neurological diseases affecting young adults. It is normally diagnosed between the ages of 20 and 40, and is about three times more common in women than men. In Australia, over 25,000 people are living with MS, with about 2.8 million people diagnosed worldwide (1).
You can jump to specific sections using the headings below.
What is Multiple Sclerosis?
MS is a chronic neurological condition that causes attacks to the central nervous system (CNS). It is characterised by inflammation and a process called demyelination (2). This is when the immune system mistakenly attacks the fatty material – called myelin – that surrounds nerve cells. Myelin is important for protecting and insulating nerves so that the electrical messages that the brain sends to the rest of the body travel quickly and efficiently. The exposed nerve cells often become scarred, which is what the term ‘multiple sclerosis’ refers to – meaning ‘many scars’.
These lesions prevent the brain from communicating messages properly, causing a range of symptoms depending on which areas of the CNS are damaged (3). This might include loss of motor function, vision changes, fatigue, and changes to thinking or memory. Each patient’s experience will be unique depending on the disease characteristics.
MS also doesn’t occur continuously, but consists of attacks, recovery, and relapses. For some people, these recovery periods will allow the nerves to regain some function. It is important to note that while MS is a lifelong condition, it isn’t terminal, and treatments can help people manage their symptoms.
Symptoms
Just like other chronic inflammatory diseases, symptoms of MS vary widely. They depend on where the lesions are and whether the person is currently experiencing an attack, or if they are recovering. Symptoms can also interact with each other and co-occurring conditions (1).
Common symptoms associated with MS – related to five major categories of functional impairment (1)
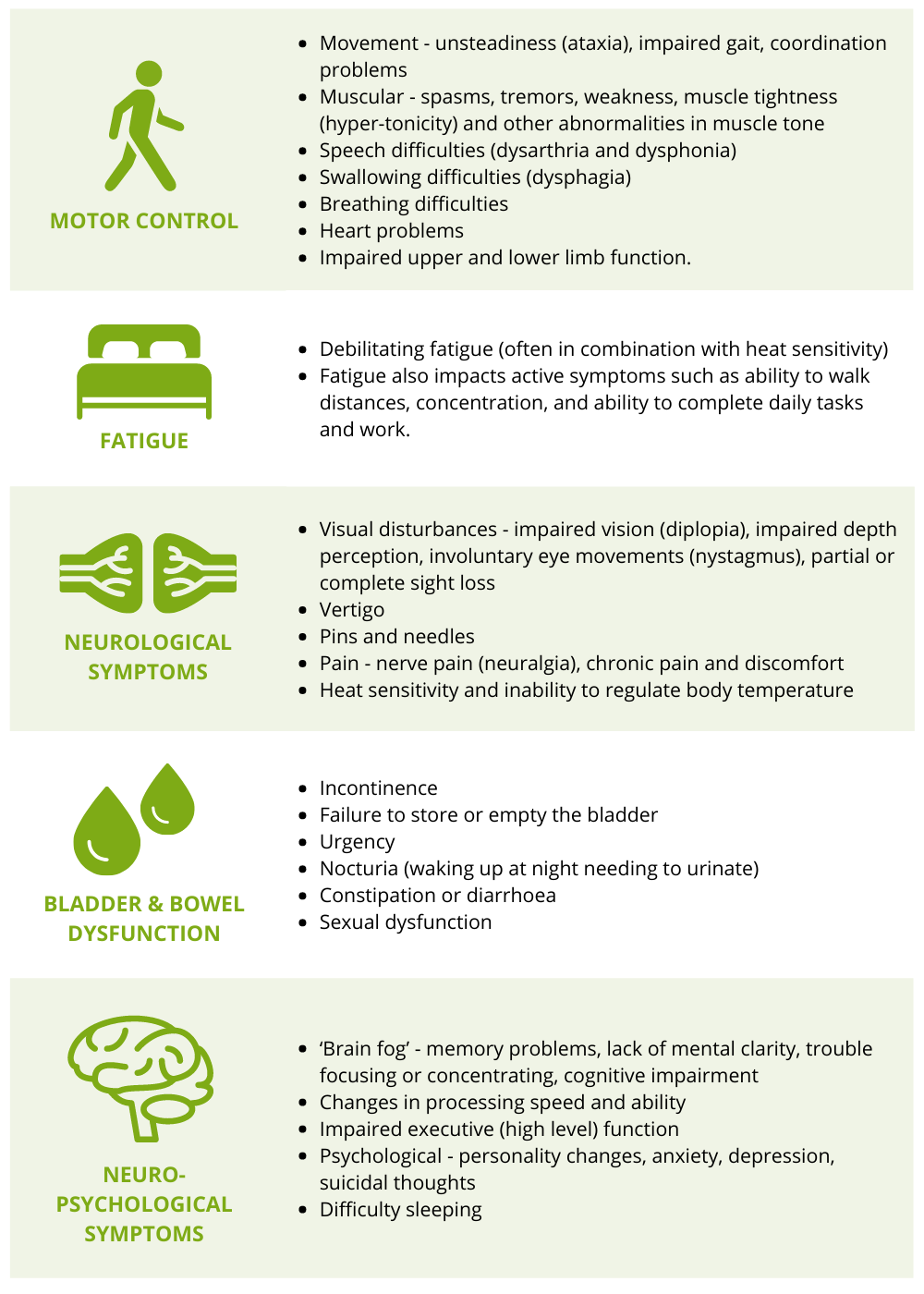
More detailed descriptions of these symptoms are available via MS Australia.
Myelin around the nerve can be repaired by the body and individuals can recover well from MS attacks. However, for some, recovery can sometimes be incomplete or symptoms can worsen over time. At this stage, people with MS might experience disability from the cumulative neurological deficits caused by the lesions.
Types of MS
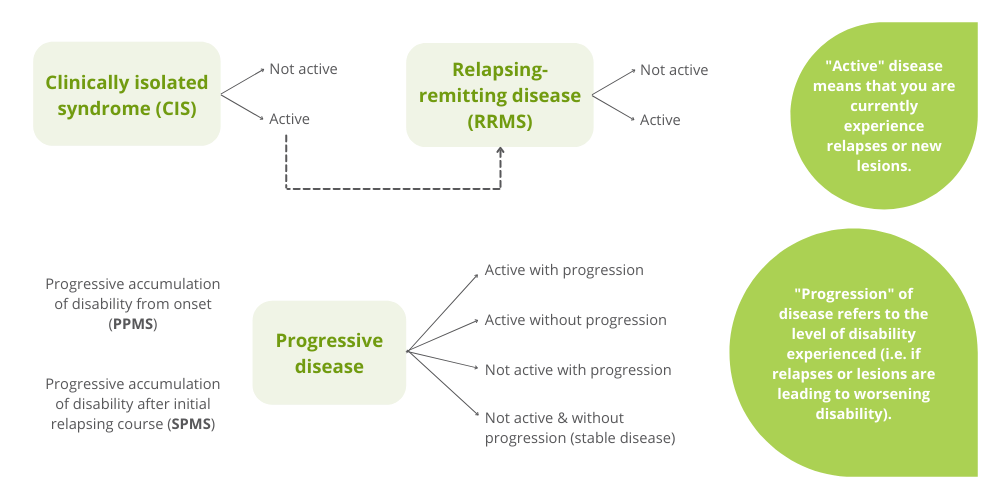
The effects and symptoms of multiple sclerosis vary greatly from patient to patient, but MS is typically classified into one of several common forms of MS.
| Relapse-Remitting MS (RRMS) | This is the most common form of MS, and usually how the disease begins. It is characterised by flare-ups of the neurological symptoms of MS, also known as relapses or attacks, followed by periods of recovery or remission. |
| Secondary Progressive MS (SPMS) | SPMS is a secondary phase of relapsing remitting MS that can develop years to decades following the initial onset of relapsing symptoms. It is characterised by a progressive worsening of symptoms (accumulation of disability) over time, with no obvious signs of remission. |
| Primary Progressive MS (PPMS) | This is diagnosed in approximately 10-15% of people with MS. PPMS is characterised by a progressive worsening of symptoms and disability right from the beginning, without periods of recovery or remission. |
| Clinically Isolated Syndrome (CIS) | A definite diagnosis of MS requires evidence for at least two attacks separated by an interval of time and/or lesions that indicate previous attacks. If there is only evidence for the current attack, then an individual may receive a diagnosis of CIS. Some people with CIS may later go on to develop MS. |
These types are more relevant from a theoretical standpoint than in clinical practice (2). A lot of the symptoms overlap, and the tests used to diagnose multiple sclerosis can’t always differentiate the subtypes. One study has suggested that MS types should have modifiers, allowing for MS to be understood as a spectrum rather than distinct categories (2). The diagram below explains how this would be used, which might help people with MS in understanding their disease state.
Causes
There is no single cause of MS, but a range of environmental and genetic risk factors have been identified as playing a role. These include:
- Genetics. Having a close relative with MS or another autoimmune disease increases susceptibility, however, MS is not a hereditary disease.
- Living further away from the equator. This is most likely related to Vitamin D deficiency, which has been linked to MS prevalence in a number of studies (1). For example, in Australia, MS is seven times more prevalent in Tasmania than it is in Queensland (5).
- Previous viral infection. Specifically, the Epstein-Barr Virus (EBV) has been linked to MS. EBV is the virus that causes infectious mononucleosis (glandular fever). Studies show that symptomatic EBV doubles a person’s chance of developing MS (6). However, it appears that the virus itself doesn’t cause MS – it could trigger some sort of immune response that predisposes someone to the disease (1).
- Smoking. Smoking increases your chance of developing MS by about 50%. It appears that the agents in tobacco smoke trigger an immune response in the lungs, which could lead to MS (6).
You can read more about the potential triggers for MS on the MS Australia website.
Diagnosis
Diagnosing MS can be difficult as patients exhibit similar symptoms to other diseases that affect the central nervous system. As yet, there is no single test to diagnose MS. However, some symptoms usually appear earlier in MS (after the first attack), which can help with diagnosis. These are often related to optic neuritis (inflammation of the optic nerve), myelitis (inflammation in the spinal cord), and brainstem or cerebellar lesions (4).
Early symptoms (1, 4)
- Fatigue
- Vision changes – blind spots or blindness, associated with painful eye movement
- Unusual sensations – pins and needles or numbness in a limb
- Incontinence
- Unsteadiness & perception issues – vertigo, stumbling, difficulty judging distances, double vision, and muscle tremors
- Slowed thinking
If your doctor suspects MS, you should be referred to an MS specialist neurologist (1). While general practitioners (GPs) or other doctors might suspect MS, only a neurologist can make a diagnosis. A neurologist that specialises in MS will also have access to the latest diagnostic criteria, treatment advice, and facilities (1). This also ensures that if there are delays in making a definitive diagnosis, you will have access to the best possible team to manage your symptoms in the interim.
Your doctor will order an MRI (magnetic resonance imaging) scan of your brain and/or spinal cord to check for areas of scarring and inflammation. An MRI is currently the most sensitive tool for diagnosing MS and excluding other conditions (2). This will be done in conjunction with other examinations, such as:
- A neurological examination to review coordination, motor skills, vision, balance, sensory, language and emotional function. This can indicate which areas of the CNS might be damaged.
- Blood tests, which help exclude other immunodeficient conditions such as syphilis or HIV-1 (6). There is also research being done to develop a blood test for MS (1).
- Lumbar puncture (spinal tap). This is often used to support MRI findings, particularly when they aren’t conclusive. If your cerebrospinal fluid (CSF) contains oligoclonal bands (OCBs), this can be used to establish if the attacks occurred at different times (which is part of the diagnostic criteria for MS) (6).
Diagnostic criteria for MS
- There have been at least two attacks at different points in time.
- More than one area of the central nervous system is damaged. The areas of damage may be evident on clinical testing, shown by MRI scanning, or electrophysiological testing.
- Other criteria, such as the presence of oligoclonal bands, are present in the spinal fluid.
For more information please see MS Research Australia’s article on the 2017 McDonald criteria for diagnosing MS.
Treatment
Currently, there is no cure for MS. However, there are a number of effective treatments called ‘disease modifying therapies’ (DMTs). These are used to slow the frequency and severity of attacks, and generally work by modifying or suppressing the immune system (7). There are also treatments used to alleviate specific symptoms of MS.
The type of DMT used depends on the MS disease type, your symptoms, and any underlying conditions (1). Because of all these factors, choosing the right DMT is best managed by a specialist MS healthcare team. This team can also provide an integrated approach to MS care, taking into account your lifestyle and monitoring your health on an ongoing basis.
For people with RRMS, the goal of treatment is to minimise relapses, and either slow or prevent them from developing SPMS. Research shows that early treatment is key at this stage, as it is more likely to prevent neurological disability and disease progression (6). Treatment can also minimise the impact of symptoms on day-to-day life and help people regain function if they were disabled by previous attacks.
DMTs available for multiple sclerosis in Australia (6, 8)
| DMT type | What does it do? | Available drugs |
|---|---|---|
| Immunosuppressants | Immunosuppressants stop the immune system from attacking the CNS, reducing inflammation and new lesions. | Fingolimod (Gilenya) Natalizumab (Tysabri) Ocrelizumab (Ocrevus) Ofatumumab (Kesimpta) Siponimod (Mayzent) |
| Immunomodulators | Immunomodulators affect how the immune system works, but do not suppress it entirely. This is more suitable for people who have a compromised immune system. | Beta interferons (Rebif, Avonex, Plegridy, Betaferon) Glatiramer acetate (Copaxone) Dimethyl fumarate (Tecfidera) Teriflunomide (Aubagio) Ozanimod (Zeposia) |
| Immune reconstitution therapy | Reconstitutive therapies are given in short courses, with the aim of providing enduring immunological changes. These drugs do not require ongoing treatment after the initial courses are completed. | Alemtuzumab (Lemtrada) Cladribine (Mavenclad) |
Many of these treatments are covered on the PBS. You can read a more detailed breakdown of these drugs on MS Australia’s website.
As with any medication, you may experience drug-related side effects and these should be discussed with your treating physician.
Symptomatic Treatments
Even though DMTs are the primary treatment for MS, there are also other drugs or therapies to help with symptom management. Symptomatic treatment might also be needed on an ongoing basis if you are experiencing functional disability between attacks.
Some treatments for specific symptoms include:
- Muscle problems (i.e. spasticity): a combination of medication may ease muscle problems, including stiffness and tremors. Some medications include Sativex or Botox. Physiotherapy is also recommended.
- Fatigue: some studies have found that medication used to treat the sleep disorder narcolepsy is helpful in controlling MS-related fatigue.
- Neurological symptoms: in some cases visual disturbances and walking difficulties can be helped with medication. Fampridine is one medication commonly used to treat walking difficulties.
- Neuropathic pain: neuropathic pain causes ‘shooting’ or burning pain due to nerve damage. This is sometimes treated with antidepressants or gabapentin.
- Continence: treatment for continence problems may include special exercises, medications, continence aids (such as disposable pads) and certain dietary changes.
- Neuropsychological problems: treatment for depression or anxiety may include counselling or medication; memory problems and other cognitive difficulties can be better managed with professional help from a neuropsychologist.
This is not an exhaustive list of symptomatic treatments. Your healthcare team will be able to create a treatment plan that suits your lifestyle and symptoms, combining pharmaceutical treatment with complementary therapies.
Prognosis
While there is no cure for MS, many people with MS live near-normal life spans. Several studies have suggested that a person with MS lives around seven years less than people without MS. Most people with MS tend to die from the same conditions that people without MS tend to die from, such as cancer and heart disease.
Most people with MS will not become severely disabled, but many experience pain, discomfort and other difficulties that can have an impact on quality of life. Medical research continues into the cause, treatments and a possible cure for MS.
Recent Research
Read Australian research papers on Multiple Sclerosis from the last 10 years.
Researcher essays about MS
Research we have funded
Dr Vivien Li – Advanced MRI To Monitor Disease Activity In Multiple Sclerosis Patients After Suspending Therapy
Dr Heidi Beadnall – research into brain tissue volume over time in MS patients
Dr Rodrigo Tomazini Martins – sleep apnoea and MS-related fatigue
Dr Sudarshini Ramanathan – identifying treatment regimes to manage blindness and paralysis in MS patients
Dr Susanna Park – associations between vitamin D and MS
Donate Your Brain
Neurological research has come away – imaging technology can show us the inner workings of our brains, and treatments can be tested on insects or mice. However, there is still a lot we don’t know, and being able to study brain tissue first-hand is a vital part of research.
People with MS in Australia can choose to donate their brain and other tissues of the nervous system for the purposes of MS research after their death. Where people have provided their consent before death, tissue is retrieved and preserved as rapidly as possible (within 24 hours) after death and stored together with the donor’s medical history.
The MS Research Australia Brain Bank facilitates MS research by distributing high quality and well-characterised MS tissue to researchers for investigating the cause of and developing a cure for MS. Registered MS Brain Donors and their families are kept up to date on the latest progress in MS research.
Researchers need to study the brain and spinal cord tissue from people with different MS subtypes and disease stages to find out how and why demyelination occurs. Researchers also need to study brain and spinal cord tissue to develop ways of repairing and preventing tissue damage.
Donating your brain to the MS Research Australia Brain Bank after your death will:
- Help researchers find diagnostic markers for early detection
- Help researchers develop better treatments
- Help researchers discover possible cures and prevention measures for MS
For more information, please call 1300 672 265, email msbrainbank@msra.org.au, or visit www.msbrainbank.org.au
See also our donate your brain page for more information about brain donation.
MS Organisations – support & advocacy
MS Australia is the national peak body for people affected by MS and is dedicated to advocacy, communications, education, funding and coordinating MS research, as part of the worldwide effort to solve MS.
There are several organisations in Australia that can provide resources, services and support to people affected by MS.
The Australian MS state organisations offer a range of support services including counselling, assessment, employer liaison, work simplification strategies, support groups, respite accommodation and much more. Services vary across organisations and locations;
There are also several organisations globally that can provide information and resources for people living with MS.
- MS Trust (UK)
- MS International Federation
- International Progressive MS Alliance
- National MS Society (USA)
- MS Society of Canada
- Multiple Sclerosis Society UK
References:
- Understanding MS, 2020, https://www.msaustralia.org.au/wp-content/uploads/2021/09/21304-msa-understanding-ms-overview-v3-final.pdf
- J Oh et al, 2018, Multiple sclerosis: clinical aspects. DOI: 10.1097/WCO.0000000000000622
- MSRA, 2021, What is Multiple Sclerosis (MS). https://msra.org.au/what-is-multiple-sclerosis-ms/
- M Olek, 2021, Multiple Sclerosis. DOI: 10.7326/AITC202106150
- S Park, 2016, Vitamin D In Neuroinflammatory Disorders. https://brainfoundation.org.au/research-grants/2015/neuromuscular-diseases-award/
- R Dobson & G Giovannoni, 2018, Multiple Sclerosis – A Review. DOI: 10.1111/ene.13819
- M Goldenberg, 2012, Multiple Sclerosis Review. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3351877/
- MS Australia, 2021, Medications and Treatments. https://www.msaustralia.org.au/about-ms/medications-and-treatments
DISCLAIMER: The information provided is designed to support, not replace, the relationship that exists between a patient / site visitor and his / her existing health care professionals.





 The Brain Foundation is the largest, independent funder of brain and spinal injury research in Australia. We believe research is the pathway to recovery.
The Brain Foundation is the largest, independent funder of brain and spinal injury research in Australia. We believe research is the pathway to recovery.