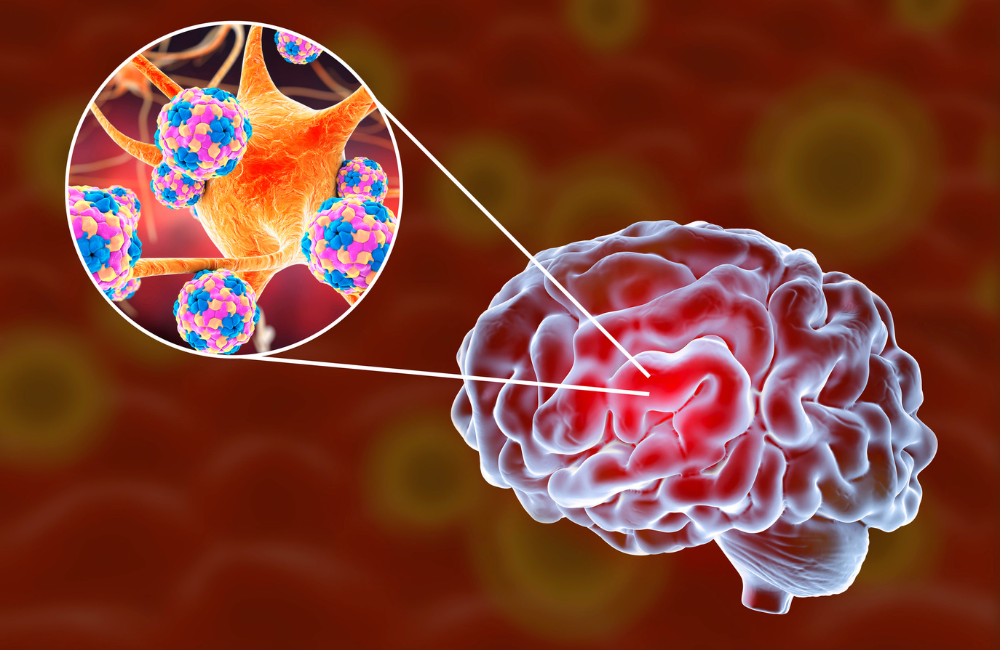
Meningitis is a rare but serious infection of the membranes that cover the brain and spinal cord. These membranes are called ‘meninges’. The infection can be caused by several types of bacteria, viruses and fungi.
Viral meningitis is usually mild and patients recover quickly. But other types can be very dangerous or possibly fatal and require immediate medical attention. Some of the distinctive symptoms to look out for include fever and a purple-red skin rash.
Click the headings below to jump to a specific section.
What is meningitis?
Meningitis is a rare but serious infection of the membranes (meninges) that cover the brain and spinal cord. It can be caused by a range of infectious causes, including infections such as bacteria, fungi, and viruses.
- Viral meningitis is usually mild and recovery is swift.
- Bacterial meningitis is a medical emergency and can be fatal without prompt treatment.
- Fungal meningitis usually progresses slowly, causing headaches and cranial nerve palsies. It may be fatal or cause permanent brain damage.
Haemophilus (Hib) meningitis used to be the most common type in Australia until a national vaccination program was set up in 1992.
Today the most common types of bacterial meningitis are caused by the Meningococcus bacteria and the Pneumococcus bacteria.
The germs that cause bacterial meningitis may live in the nose and throat. People of any age can carry them without becoming ill, but they can infect someone else through coughing or sneezing.

Symptoms in small children & babies:
- Fever
- Yellow skin (jaundice)
- A bulge in the soft spot on the top of the head (the fontanelle)
- Unusual or high-pitched crying
- Fretfulness or irritability
- Inactivity and floppiness
- Food refusal
- Being difficult to wake
- Purple-red skin rash
- Pale or blotchy skin
- Seizures (fits)
Symptoms in older children & adults:
- Fever
- Very bad headache
- Neck stiffness and joint pains
- Sensitivity to light
- Nausea or vomiting and loss of appetite
- Tiredness and drowsiness
- Irritability or confusion
- Purple-red skin rash or bruising
- Seizures (fits)
You won’t necessarily experience every single symptom if you develop meningitis. If you are concerned you should contact your GP immediately. If your doctor is not available, go to the emergency department of your nearest hospital.

Causes of meningitis
Viral infections are the most common cause of meningitis, followed by bacterial infections. These types of meningitis are often spread by coughing, sneezing, or close contact such as kissing.
- Viral meningitis is usually caused by enteroviruses (common stomach viruses). It can also be caused by the West Nile virus, mumps, measles, herpes simplex types I and II, chickenpox, and lymphocytic choriomeningitis (LCM) virus.
- Bacterial meningitis can be caused by meningococcal, pneumococcal, haemophilus influenzae type B (Hib), tuberculosis, group B streptococcus and E.coli meningitis bacteria.
Fungal and parasitic causes are very rare. They are a bit different from viral and bacterial meningitis, as they cannot be spread from person to person.
- Fungal meningitis is more likely to affect people with weakened immune systems (i.e. due to cancer or HIV). It is most commonly caused by a fungus called Cryptococcus.
- Parasitic meningitis can be caused by a few different parasites. Many of these typically infect animals, and are passed onto humans through contaminated food. There is also a rare parasitic amoeba found in lakes, rivers or ponds, which can cause a particularly life-threatening infection.
While each of these types of meningitis have different causes, they ultimately work in the same way. The bacterium, virus, fungus, or parasite spreads through the body until it reaches the brain or spinal cord. It then develops into a more advanced infection.
Risk factors
There are a few different risk factors that increase your susceptibility to meningitis. These include:
- Skipping vaccinations. There are several vaccines available to prevent some of the viruses and bacteria that cause meningitis. Make sure you are up to date with these vaccinations to reduce your risk.
- Living in a community setting. Bacteria and viruses can spread quickly when large groups of people live in close quarters, such as boarding schools, camps, child care facilities, military bases, etc.
- Age. Most cases of viral meningitis occur in children under 5 years old. Bacterial meningitis is common in people under 20 years old.
- Pregnancy. Pregnancy increases your risk of infection with listeria, which can cause meningitis. Listeria may be present in soft cheese, raw seafood, cured meats, and some other foods.
- Weakened immune system. Any factor that compromises your immune system can increase your risk of meningitis. This includes HIV/AIDS, autoimmune disorders, diabetes, cancer, chemotherapy, and more.
Prevention & vaccines
You can reduce your risk of meningitis by maintaining good hygiene. It is important to wash your hands regularly, dispose of used tissues immediately, and avoid sharing food or drinks.
However, one of the best ways to prevent meningitis is to get vaccinated. There are several vaccines available in Australia to protect against meningococcal, but no one vaccine protects against all subgroups of the disease.
- Two vaccines protect against meningococcal serogroup B – Bexsero and Trumenba
- Two vaccines protect against meningococcal serogroup C only – NeisVac-C and Menitorix
- Three vaccines protect against meningococcal serogroups A, C, W and Y – Nimenrix, Menactra and Menveo
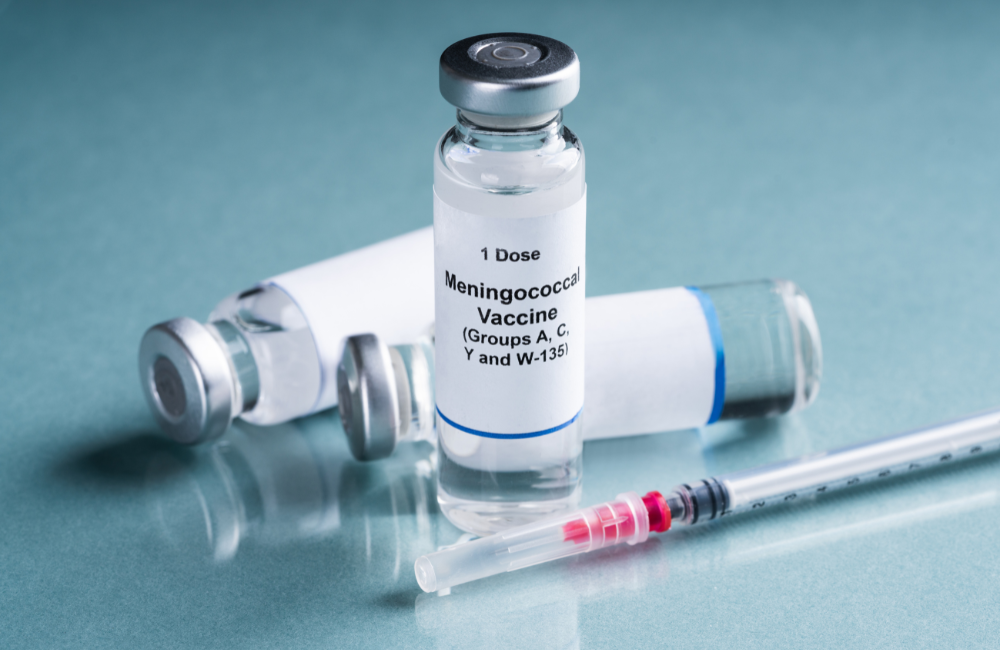
You can access some of these vaccines for free under the national immunisation program. The ACWY vaccine is free for children aged 0-12 months and adolescents aged 14-16 years through school-based vaccination programs. The meningococcal B vaccine is free for Aboriginal and Torres Strait Islander children aged 2 months, 4 months, 6 months (certain medical conditions) and 12 months. Both of these are also free for people of all ages with asplenia and hyposplenia, complement deficiency and those receiving treatment with eculizumab.
You can read the full eligibility criteria and more information about the vaccination program on the Department of Health website.
Diagnosis
If you have symptoms of meningitis, your doctor will often ask you about your medical history, take a blood test, and sometimes perform a lumbar puncture (spinal tap).
Questions about your medical history and lifestyle can be important in diagnosing what type of meningitis you have. For example, a person living in a university dormitory is more likely to have a bacterial infection, while someone working on a farm could have been exposed to a parasite.
A blood test and spinal tap allow doctors to confirm the type of meningitis and the exact cause of the infection. They may also use imaging to scan your brain or lungs to identify the extent and/or origin of the infection.

Treatment for meningitis
Viral meningitis is usually mild and antibiotics are not needed. It is usually treated like the flu with patients advised to get bed rest and drink plenty of fluids.
Bacterial meningitis is a medical emergency and can be fatal if not treated quickly. Intravenous antibiotics are usually started as soon as bacterial meningitis is suspected. Close contacts are sometimes given clearance antibiotics to reduce the risk of further infection.
Fungal meningitis is treated with intravenous and oral antifungal agents. However, antifungal treatments can have negative side effects, so treatment is often delayed until test results confirm that the cause is fungal.
Prognosis
Prompt treatment of meningitis is vital. Early diagnosis and treatment reduce the risk of infection and the risk of complications from infection.
Viral meningitis is usually mild and recovery is swift with the illness getting better on its own in 7-10 days.
Bacterial meningitis can be severe. Recovery can be slow and not everyone has a full recovery.
In serious cases meningitis can cause permanent disability or even death. The death rate is about 5 percent. The longer a person has the disease without treatment, the greater the risk of permanent neurological damage, such as:
- Hearing loss
- Memory problems
- Learning disabilities
- Brain damage
- Trouble walking
- Seizures
- Kidney failure
Further information & resources
If you would like to learn more about meningitis, you can explore the following articles, resources, and support organisations:
- Read the latest Australian research papers on meningitis via the National Library of Medicine >
- Meningococcal disease – our article about meningococcal, which is one cause of meningitis
- Article from the National Institute of Neurological Disorders and Stroke (USA)
- HealthEngine article
- Meningitis Centre Australia – Australian support organisation
- Confederation of Meningitis Organisations – a global network of organisations and individuals dedicated to defeating meningitis globally
DISCLAIMER: The information provided is designed to support, not replace, the relationship that exists between a patient / site visitor and his / her existing health care professionals.





 The Brain Foundation is the largest, independent funder of brain and spinal injury research in Australia. We believe research is the pathway to recovery.
The Brain Foundation is the largest, independent funder of brain and spinal injury research in Australia. We believe research is the pathway to recovery.